

The Proactive Assessment Unit (PAU) enables NHS patients to have their care needs to be professionally assessed in a caring, friendly and homely environment without remaining in an acute hospital bed.
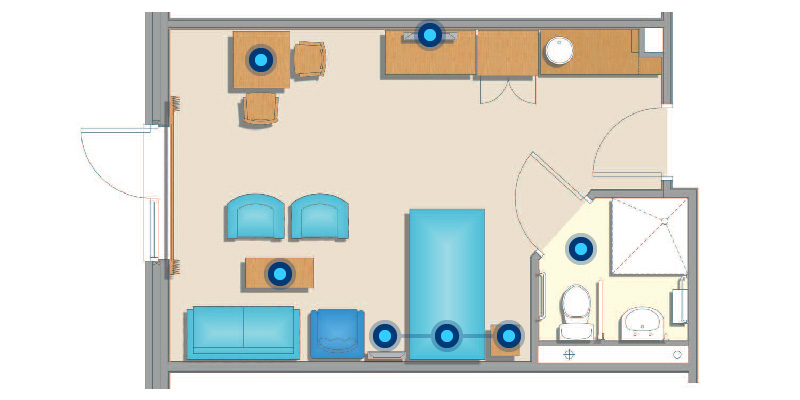
Click the buttons on the diagram below.
Our Statement of Purpose will tell you about the Home, our aims and objectives, together with our philosophy of care. It also includes a description of the services and facilities on offer at the home.